GENERAL
Effective Strategies for Maintaining Long-Term Sobriety

Maintain long-term sobriety by developing a solid support network, attending regular therapy or support group meetings, and adopting healthy lifestyle habits. Identify and manage triggers, set achievable goals, and practice stress-relief techniques. Prioritize self-care, stay accountable, and celebrate milestones to sustain motivation and prevent relapse.
Introduction
Sobriety is a journey marked by numerous challenges and triumphs. Participating in AA Classes Near Me is a decisive step toward long-term recovery for many. However, it’s crucial to complement this with other effective strategies to maintain sobriety over time. Nobody embarks on this journey alone; a combination of personal effort and external support can pave the way to a fulfilling, addiction-free life.
Long-term sobriety requires a multifaceted approach. Understanding your triggers, building a supportive network, establishing healthy routines, practicing mindfulness, and seeking professional help are all fundamental strategies that contribute to sustainable recovery. Let’s explore each of these aspects in detail.
Understanding Triggers
Recognizing the situations, feelings, and people that can lead to relapse is vital in maintaining sobriety. By identifying these triggers, you may create plans to handle or avoid them. Triggers can be external, such as specific environments or social settings, or internal, such as emotions or mental states.
Common Triggers
- Stress from work or personal life
- Social situations involving alcohol or drugs
- Emotional states such as loneliness or depression
- Significant life changes, like moving or changing jobs
- Anniversaries of significant dates related to past substance use
Research suggests that having a plan in place and being aware of these triggers can greatly lower the chance of relapsing. For instance, learning stress management techniques or avoiding social gatherings where alcohol is present can be effective strategies. Self-awareness is the first step toward change, and recognizing what triggers your cravings can empower you to take control.
Building Support Networks
A robust support system is critical for maintaining long-term sobriety. This network can include friends, family members, and support groups like Alcoholics Anonymous (AA). Studies show that people with a robust network of support are more likely to stay sober for more extended periods. The emotional safety net these support systems provide can be invaluable in times of stress or temptation.
Benefits of Support Networks
- Emotional support and a shoulder to cry on during trying times
- Accountability partners to keep you on track and honest about your progress
- Opportunities to share experiences, advice, and coping strategies
- a feeling of camaraderie and belonging that lessens feelings of loneliness
- Access to resources and information for continued recovery efforts
Building and maintaining these relationships provides the emotional and psychological support necessary for sobriety. Whether through organized groups like AA or informal gatherings of friends and family, having a reliable support system is crucial. Loneliness can be a significant trigger for relapse, so maintaining social connections can be a buffer against returning to old habits.
Establishing Healthy Routines
Establishing and following a daily schedule might be essential to sustaining sobriety. Incorporating healthy habits like predictable sleep schedules, balanced diets, and frequent exercise may give your life structure and stability. Routine provides you with constructive tasks to focus on, filling the hole created by substance abuse.
Components of a Healthy Routine
- Engage in regular physical activity, which boosts mood and health
- Maintain a balanced and nutritious diet, ensuring your body gets the necessary nutrients
- Ensure you get at least 7-8 hours of sleep every night to promote your physical and emotional health.
- Set specific goals for daily activities, providing a sense of accomplishment and direction.
- Include time for hobbies and interests that keep your mind engaged
Get at least 7-8 hours of sleep every night to promote physical and emotional health. Exercise releases endorphins, known as “feel-good” hormones, which can be particularly beneficial in managing mood and stress.
Practicing Mindfulness
Mindfulness and meditation can be incredibly effective for managing cravings and staying grounded. By focusing on the present moment and acknowledging feelings without judgment, you can handle stress and triggers more effectively. By encouraging a clear and composed mind, mindfulness aids in ending the loop of unfavorable ideas and actions.
Practices for Mindfulness
- Meditation techniques to calm the mind
- Breathing exercises to manage stress and anxiety
- Yoga to improve both mental and physical health
- Mindful eating, which encourages savoring each bite and recognizing hunger and fullness cues
- Mindful walking, focusing on the sensation of walking and breathing
An article from Psychology Today highlights various mindfulness practices and their benefits, emphasizing the importance of consistently practicing these techniques for optimal results. Mindfulness can be integrated into daily life, providing a tool to manage the ups and downs of recovery without resorting to substance use.
Seeking Professional Help
The road to recovery can sometimes require professional intervention. Therapists, counselors, and healthcare professionals can offer personalized guidance tailored to your needs. Cognitive Behavioral Therapy (CBT), for example, is an evidence-based approach that focuses on altering unhealthy patterns of thought and behavior. Professionals can provide a different perspective and tailored strategies that might not be apparent to you.
Benefits of Professional Help
- Individualized care regimens created to address your unique requirements
- Expert advice and support from trained professionals
- Evidence-based therapeutic techniques such as CBT or Dialectical Behavior Therapy (DBT)
- Monitoring of progress and adjustments to treatment plans as needed
- Access to medical treatments and medications that can aid recovery
If managing sobriety becomes difficult, seek professional help. Therapists and healthcare providers can offer new coping mechanisms and address mental health issues. Sobriety is a lifelong commitment requiring continuous effort and support. Understanding triggers, building a support network, maintaining healthy routines, practicing mindfulness, and seeking professional help can help you navigate the complexities of sobriety and lead a fulfilling, addiction-free life.
GENERAL
Tips for Hosting Gatherings in Your Townhome

In contemporary townhomes, hosting capacity depends on how the space is designed and equipped. Structural features, room layouts, and interior upgrades influence how many people the home can accommodate. Open layouts, integrated storage, and multi‑use furniture expand usable hosting space without increasing square footage. Here are tips for hosting gatherings in your townhome:
Optimize Living Spaces
In most townhomes, storage is built into the building itself, which minimizes clutter and maximizes available square footage for hosting gatherings. Larger groupings of furniture are possible without any structural modification due to open-plan areas of living and dining. Lighting through recessed ceilings enhances brightness and does not require large floor lamps.
Wall-mounted TVs and shelving help free up floor space for extra tables or seating. Upgraded flooring options like engineered wood or luxury vinyl can handle higher foot traffic. Wide doorways between the living and dining spaces improve circulation while remaining open without doors. Bright lighting allows homeowners to easily control different areas without extra wall switches. Collectively, these features create a more adaptable central hosting area.
Flexible Furniture Layouts
In contemporary townhomes, modular furniture designs enable layout changes without moving the large permanent items. Sectional couches with removable pieces facilitate various sitting arrangements. You can expand surface area with extendable dining tables that only appear when you need more space.
Nesting tables provide a temporary storage option and are able to be compactly stored when not in use. In storage ottomans, seating and hidden storage are combined as one upgrade. Folding tables attach to walls, offering extra surfaces without taking up floor space. Composite materials are lightweight, allowing homeowners to easily rearrange them to suit different layouts. These upgrades support various hosting styles without the need for remodeling.
Design Activity Zones
Open-concept townhomes feature architecture that subtly separates spaces without enclosing them. Kitchen islands serve as natural dividers between food preparation and social zones. Lounge and dining areas are visually distinguished by half-walls or built-in shelves. Area carpets define seating zones in high-traffic parts. Overhead track lighting highlights specific areas within common rooms. Sliding glass doors create a division between indoor and outdoor spaces while allowing natural light to flow through. Smart home zoning enables independent control of lighting and audio in different areas. These design elements maintain organization without sacrificing openness.
Develop a Plan Noise
In a carefully designed townhome, effective sound control begins with material and layout selections. Using sound-absorbing wall panels reduces echo between connected living areas. Double-pane windows help block exterior noise and contain interior sounds. Wider staircases and corridors facilitate easier movement across floors. Open railings promote a more even sound distribution than solid walls. Thoughtfully placed doors reduce traffic congestion around seating areas. These improvements boost mobility and sound management during gatherings.
Find Townhomes for Rent
Successful townhome hosting depends on design characteristics and physical enhancements instead of transient setup modifications. Adaptable interior spaces are formed by storage integration, modular furniture, and open layouts. Wall treatments, flooring, and lighting systems enhance durability and visualization. Browse townhomes for rent.
GENERAL
How to Choose Among Helium SEO & Other San Diego Companies

Succeeding in today’s business landscape certainly requires you to, well, play the online game. In other words, if you really want to make it on today’s market, you will have to go digital. Consumer behavior has changed quite a lot, and nowadays, everyone is turning towards online shopping, or at least researching companies online before they contact them, which means that you have to have online presence in order to grab attention and build your brand.
Now, as I’m sure you understand already, there are various different strategies that you can use to your advantage when wanting to build great online presence and stand out from the crowd. And, of course, search engine optimization is one of those. Standing out for the long-term results it brings, the organic traffic, conversions, and various other things, SEO is undeniably a strategy that you have to invest in nowadays. Once again, though, I’m sure you understand that already.
Just like you get the significance of working with professionals to make things happen for yourself. To put it simply, if you want to grow your San Diego business, you will absolutely have to hire a great San Diego SEO company to help you achieve your goals. And, if you’ve been doing any kind of research already, then you may have come across Helium SEO and similar experts, which has made you wonder.
To cut right to the chase, you’re wondering how to choose among those different companies you have come across. After all, Helium SEO and other firms cannot all be the same. So, what you want to do is figure out how to actually choose among them and be happy with the hiring decision you have made. And, well, that’s what we’re going to cover in this article, so keep on reading to find out what you need to know.
Define Your Business Goals
Clearly, before you can make any kinds of choices, you will have to define your goals first. After all, to choose an amazing San Diego SEO Company, you will have to choose on that aligns with your goals, and that knows how to help you meet them. So, think about whether you want to rank locally, grow nationally, increase organic traffic, boost ecommerce conversions, build brand reputation, or do all of the above and more. Defining your goals is sure to help you ultimately make the right choice.
Set Your Budget
Moving on, you will also have to set your budget. Helium SEO and other companies are all bound to charge different amounts of money for their services. This is completely normal. But, in order to choose the firm that is right for you, as well as the range of services that you will be able to afford, you will certainly have to set your budget before making any kinds of agreements with any of the professionals you will come across.

Compare Specific Experience
Another thing you should do, of course, is check and compare the experience levels of Helium SEO and any other companies you may be considering. After all, you want to make sure that you are getting the most out of the professionals, and in order to make that happen, you will need to choose highly experienced companies to do the work for you. But, I am not talking simply about general SEO experience.
What I am also talking about is the specific experience in your particular industry. As well as local experience. So, keep those factors in mind when assessing any of these professionals, as that is bound to help you make the right choice at one point.
Read some more about SEO for your branding: https://pmc.ncbi.nlm.nih.gov/articles/PMC11066527/
Compare Reputation Too
Of course, comparing the reputation of Helium SEO and all the other firms you may be considering is also an important thing to do when trying to make the best choice here. After all, you want to choose highly reliable professionals to provide you with the services you need. So, read some reviews on all of them and compare the reputation before deciding on anything.
Interview Different Candidates
Interviewing different candidates is, without a doubt, another thing to do before making a hiring move. So, talk to Helium SEO and some other companies you believe may be right for you. Ask any questions you may have, talk about the potential strategies, and generally assess the quality of communication.
Check Out Case Studies and Results
Finally, take some time to check out the case studies provided by different companies, as well as the results. This will help you get a better idea about the quality of work to expect from certain professionals. And, there is absolutely no denying the fact that you want to choose those experts that have been providing their clients with great quality work.
GENERAL
Landscape Project Planning That’s Made Effortless
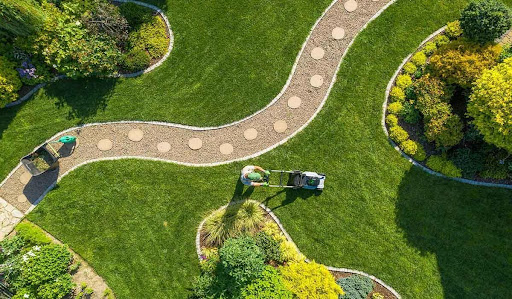
Homeowners would often want to start an outdoor project, but it’s hard to balance the ideas with the steps that are needed to make this happen. Those who live in the cities might have unpredictable tight schedules, and they don’t generally have the time to drive to different nurseries to get the materials that they need, like stones.
Fortunately, a reliable company that specializes in delivering stones can help them turn their vision into a reality. The homeowners can simply arrange for the shipping of the stone, and they don’t have to burden themselves with the transport.
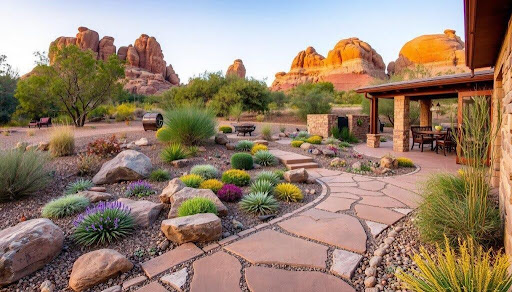
Selecting stones as one of the major design elements can open up a lot of possibilities in a landscaping project. The ones from Chicago decorative stone delivery can combine a lot of styles with specific structures to sharpen the look of a home’s walkway. The polished pebbles may also add some texture in a garden bed so the entire yard can look more refined regardless of the season.
Understanding Stone Types Before Starting a Project
Many homeowners prefer river rocks that can be great additions to water features, and they can enhance the natural look of a garden. There’s minimal maintenance needed with them, and they can easily be shifted.
Crushed stones are angular types that are commonly utilized in driveways, and they offer stability because of the jagged edges. They’re more affordable, especially if one wants to cover a large area, but they may be uncomfortable to walk on barefoot.
Limestones are flat, and they can add a high-end feel to landscaping. However, these are expensive and require a proper base before the installation, so they don’t shift. There are a lot of other options, and it’s important to know more about the different varieties available to avoid mismatches.
Project Layouts That Benefit from Stone
Small yards can be transformed through well-placed stone accents like borders in garden beds. They can also add a definition that contains the soil. Gravel that you can read more about here and are added to walkways can also reduce mud during rainy seasons, and it adds texture that can complement greenery.
For a larger yard, this can mean more room for innovation, where homeowners can create distinct zones like fire pit spaces. This becomes easier when the stone can outline some sections, and it cleans the edges to guide the flow of traffic in a property.
Boost Curb Appeal with Subtle Enhancements
Oftentimes, the look of a garden can set the tone for the home, and this is where decorative stones can bring harmony to an entryway. It can make the overall look become more thoughtfully arranged, and you can pair them with native plants. The right pebbles are versatile, and they will result in an aesthetically pleasing rhythm without being excessive.
This can be a long-lasting solution for areas near the borders that don’t receive too much sunlight. These stones are not going to break down quickly, so it’s great for homeowners who want materials that are low-maintenance.
Use Stone to Improve Garden Efficiency
The stones are going to contribute more than beauty, and they can help the project become a long-term success. Use several of them to help with the drainage to prevent soil erosion in the yard, and they can become valuable in climates where unpredictable storms are present.
Gardeners in Chicago may also use the pebbles as barriers to keep the invasive plants at bay. They can keep the different soil types separated from each other for healthier plant growth, and this is going to be a dependable choice for those who want a long-lasting landscape.
Blend Stone with Plants for Natural Harmony
Buying stones for your project in Chicago can mean that you’ll have a well-balanced outdoor space where the bushes can soften the strong edges of the pebbles. Grasses can gently sway beside the gravel paths, and the flowers can look striking when you add the darker stones.
Getting the materials that you need can set the tone of your garden, so it becomes more cohesive. Choose warm-colored options if you want to complement your foliage with earthy tones, while the cooler shades can be great for purples.
Enjoy Door-to-Door Deliveries Today with the Materials You Need
Transporting the heavy stones often requires a lot of physical effort, not to mention other resources like time. Fortunately, there are dependable delivery companies in Chicago that can speed up these orders with lead times between 24 and 48 hours. You can avoid doing multiple trips to various nurseries and simply click your preferred order and wait for it to arrive.
It’s very efficient for those who are too busy with their jobs but want a beautiful garden, nevertheless. You can also free up energy towards building your garden instead of doing all the heavy lifting. Call these companies today to get high-quality natural stones that can last for decades.
-

 GENERAL2 years ago
GENERAL2 years agoDiscovering the Artistic Brilliance of Derpixon: A Deep Dive into their Animation and Illustration
-

 Posts2 years ago
Posts2 years agoSiegel, Cooper & Co.
-

 HEALTH2 years ago
HEALTH2 years agoTransformative Health Solutions: Unveiling the Breakthroughs of 10x Health
-

 Lifestyle2 years ago
Lifestyle2 years agoPurenudism.com: Unveiling the Beauty of Naturist Lifestyle
-

 FASHION2 years ago
FASHION2 years agoThe Many Faces of “λιβαισ”: A Comprehensive Guide to its Symbolism in Different Cultures
-

 Lifestyle2 years ago
Lifestyle2 years agoBaddieHub: Unleashing Confidence and Style in the Ultimate Gathering Spot for the Baddie Lifestyle
-

 Entertainment2 years ago
Entertainment2 years agoGeekzilla Podcast: Navigating the World of Pop Culture, Gaming, and Tech
-

 Lifestyle1 year ago
Lifestyle1 year agoSandra orlow: Unraveling the Story of an Iconic Figure
